Abstract

Introduction: Combination of doxorubicin, bleomycin, vinblastine and dacarbazine (ABVD) is the standard of care in frontline therapy for classic Hodgkin lymphoma (cHL). Since 2018, bleomycin shortages have been reported in Brazil, with severe consequences for cHL patients. In the private setting, many institutions chose to use A+AVD, in which bleomycin is replaced by brentuximab-vedotin, or to import bleomycin from vendors not registered at the national drug agency. For public institutions, however, these costly strategies are largely unattainable.
Methods: We conducted a single-arm open-label study to evaluate the substitution of bleomycin with etoposide 100 mg/m2 on days 1 and 15 of every 28-day cycle (AEVD) in previously untreated cHL, at Hospital Municipal São José, in Joinville, Brazil. Here we present preliminary data on the safety and efficacy of this combination in a scenario of lack of approved treatment options for this patient population.
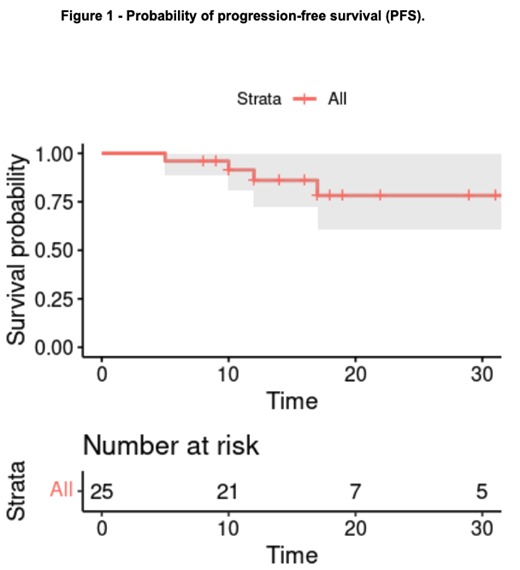
Results: Twenty-five patients aged 18 or more with cHL diagnosed between June 2018 and November 2020 were included. Fourteen patients (56%) were male, with median age of 27 years (range: 18-66). Most patients were stage II (60%, n=15), presented with B symptoms (56%, n=14) and high lactate dehydrogenase (LDH, n=13, 52%). For stage III-IV (n=5), high-risk IPS was present in 3 patients (score >2; 60%). For localized disease (n=20), unfavorable features according to the GHSG were seen in 16 patients (n=80%). All patients received between 3 and 6 chemotherapy cycles, with no recorded adverse event requiring hospitalization, treatment interruption or discontinuation. PET-CT was performed solely outside of our institution. Eight patients had access to interim PET-CT, all with Deauville scores (DS) 1-3. Overall response rate was 96%, with one disease progression after 5 cycles. Seven patients had CT scan-alone end-of-treatment (EOT) assessment, with 5 complete responses (CR) and 2 partial responses (PR), with both PR patients sustaining remissions after 10 and 12 months. EOT assessment with PET-CT (n=18) resulted in DS 1-3 in 72% (n=13), 4 in 22% (n=4) and 5 in one (6%). All 5 patients with DS 4-5 underwent biopsy after EOT assessment, with confirmation of relapsed or refractory (RR) cHL in 4 cases (22 year-old, stage IV high-risk female with progressive disease; 65 year-old, stage III low-risk male with relapse 11 months after EOT; 26 year-old, stage II high-risk male with relapse 6 months after EOT; 25 year-old, stage II high-risk female with relapse 4 months after EOT). Two RR cHL patients (50%) had treatment delays exceeding 30 days due to psychosocial or financial impacts emerging from the COVID-19 pandemic. All RR cHL patients had access to salvage treatments. At a median follow-up of 16 months (range: 8-36), no death was recorded and 12-month progression-free survival probability was 86% (95%CI: 72%-100%).
Conclusions: Drug shortages impacting chemotherapy treatments have been a recurring problem worldwide, most noticeably among cytotoxic agents without in-class validated substitutions, as is the case with bleomycin. AEVD, as a novel approach to newly diagnosed cHL, appears to be safe, feasible and highly active in a population composed mostly of high-risk patients.
Boettcher: Novartis: Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal